It has become clear that the wants and needs of nephrology fellows looking for employment in general, and specifically in the private practice sector, have changed in the past 40 plus years that I have been recruiting in the profession.
When I first started, the primary objective of a fellow coming out of training was to either start a practice with the assistance of an income guarantee sponsored by a local hospital (to help establish themselves in a community) or to join an existing practice with the idea of becoming a partner.
Nephrology is not an easy specialty to master – a chronic illness like end-stage kidney disease can make patient management challenging and time-consuming. That was understood if you joined this profession as a fellow years ago.
Today and for the better part of the past decade, work/life balance has become the major priority to fellows when discussing practice opportunities. It is not limited solely to nephrology; it is a priority with fellows in other specialties and probably for many people entering the workforce in general. A survey conducted by the American Psychological Association in 2023 showed that 92% of workers reported working for an organization that values their emotional and psychological well-being is very or somewhat important.
According to results from the 2022 Nephrology Fellows Survey published by the American Society of Nephrology, the top four factors influencing a fellow’s decision in considering an employment offer (rated either extremely or very important to the fellows interviewed) were weekend call frequency, overnight call frequency, desired location and workday length. These were followed closely by predictable workday and compensation.
Demanding specialty
The problem the nephrology world faces is that work/life balance and practicing nephrology in a private practice setting are counterintuitive. A shortage of nephrologists since the start of the specialty has always put extra workloads on those practicing. Remember the projections of potential patients and costs in 1972 when Congress approved Medicare for dialysis payment? Legislators did not anticipate that the Medicare entitlement would grow to treat older, sicker patients and assumed younger patients would all get transplants and go back to work. Twenty-five years later in 1997, it was clearly stated again in an ad hoc committee report co-written by representatives of various nephrology and transplant associations, including the ASN and the Renal Physician Association.
Today, partly through Medicare funding aimed at slowing the progression of chronic kidney disease, the annual growth in the number of patients with ESKD has slowed (the high mortality rate among patients with kidney disease who contracted COVID-19 also depleted the prevalent population).
According to quarterly updates released by the U.S. Renal Data System, 136,196 patients were newly diagnosed with ESKD in 2021. That number decreased to 131,216 in 2022 and, if the pattern of quarterly counts continues, new cases will be approximately 130,930 in 2023.
Still 808,000 prevalent patients had ESKD in the United States at the end of 2021. More significantly, more than 37 million Americans have some form of CKD. Back in 1997, when the ad hoc committee report was released, the ESKD population was less than 300,000. The total nephrology physician population at that time was around 4,800; today it is closer to 12,600.
Attracting fellows
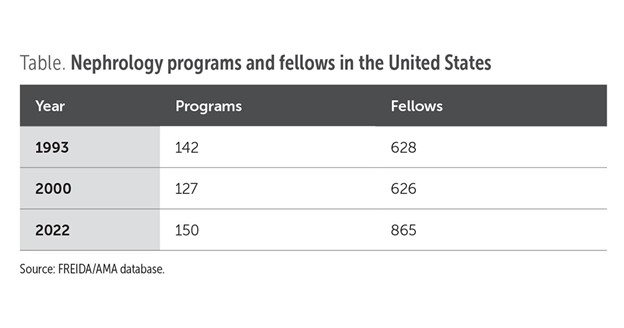
The nephrology community has tried to address these numbers by expanding the number of fellowship programs and the number of fellows completing those programs (see table).
Even with the additional programs today, the most recent match results are alarming: Overall, 52% of the training tracks for nephrology (of which there are 180) filled completely. Likewise, 66% of positions in those tracks were filled (321 of a possible 488 nephrology open positions).
While better than fill rates during 2010 to 2019, the numbers have been trending downward since 2020. Of the major internal medicine specialties, the majority achieved fill rates in the 2024 match in excess of 95%. Nephrology joined geriatrics and infectious disease at less than 66%.
Why does this happen? Internal medicine residents going through rotations in nephrology see that nephrologists tend to manage the sickest of patients, work longer hours and have the added component of having to go to visit patients in dialysis facilities (in order to collect the monthly capitated payment) in addition to maintaining an office and hospital practice. The complexity of the specialty and the stress and ramifications of decisions is not always something that all residents want to deal with. Compensation is an issue as well.
Looking at the most recent Physician Starting Salary Survey put out by the Medical Group Management Association, the mean starting salaries for nephrologists first year post fellowship were the fifth lowest among 60 specialties reporting. The median starting salary ranked better but was still in the lower 25th percentile.
While the sample size for this survey is small, it can be used conceptually to compare with other specialties. Somehow, the nephrology community must do a better job of increasing these starting numbers to help attract residents to the specialty.
Changes in productivity
Nephrology is impacted by all these factors: the shortage, the long hours, complexity/difficulty of the specialty, and the lower compensation. Also, for a multitude of reasons, those fellows are not going to be as productive as those physicians already in practice. In a recent interview in NEJM Catalyst, Daniel Varga, MD, chief physician executive for Hackensack Meridian Health System, said, “The problem is that the ones (doctors) they’re replacing are two X of them, and we’re going to have to figure how to redesign the care model in a way that allows those doctors to be the good doctors they are, but at the same time provide the same access to care that we’re providing today, if not more.”
He goes on to describe this as a generational change — a good change but one that needs to be addressed. It is not just a matter of replacing bodies, it is a matter of replacing productivity.
To facilitate work/life balance in nephrology, all these issues need to be dealt with. Some options include the following:
The recent advancements seen with AI also have the potential to be a game changer; however, its use must be approached cautiously. AI “presents unprecedented opportunities to enhance patient care, improve diagnostics, streamline workflows and facilitate more precise treatment decisions ... [it] can also be used in the applications in diagnosis, risk prediction, treatment optimization and patient monitoring,” Francesco Bellocchio, MD, PhD, and colleagues wrote in Frontiers in Nephrology. “While the potential of AI in nephrology is immense, its implementation comes with challenges and ethical considerations.”
Without making changes, the specialty of nephrology will continue to have difficulty attracting new fellows and meeting the needs of the kidney community.
With the most recent delta variant – and the potential for others to follow – the coronavirus has made hospitalization rates and high death tolls a way of life.
There is nothing in the foreseeable future that makes one believe things will get back to normal anytime soon, and that has had an impact on the nephrology workforce.

As has been previously documented in numerous articles and reports, the nephrology workforce has had a shortfall of physicians going into the specialty for several decades. Besides the usual explanations – low pay compared with other medical specialties, dealing with a complex and chronic disease, too much time between multiple offices, dialysis units and hospitals, and long hours – the fact is fewer residents are going into this specialty.
Nephrology has one of the lowest match rates of any subspecialty and has the lowest pass rates for any subspecialty board after completion of training.1 The biggest impact, however, on workforce is fewer fellows coming out of training are going into private practice.
Utilizing the Fellowship and Residency Electronic Interactive Database, which is managed by the AMA, it is evident that private practice in nephrology does not hold the same appeal as it did 10 years ago. The percentage of fellows completing training who chose who choose private practice has gone down substantially from 70.3% in 2011 to 45.9% in 2020.2 Although these numbers are not absolute (only 87.3% of fellows reported their plans in 2020), the figures provide a good indicator of the decrease in private practice interest.
COVID-19 further exacerbated these issues. Data are hard to come by, as many of the usual resources that track trends in fellowship training have been delayed or canceled during the past 18 months. The following is what we do know for most of the second and third quarters of 2020:
Zoom, Skype or FaceTime meetings quickly became the tool of choice to interview for jobs. These work well if candidates are familiar with the geographic area where they are interviewing but do little to introduce them to a new community where they may be looking to spending the next part of their lives.
For the fellows coming out of medical school in June 2020, most of them knew where they were going 4 months earlier (when lockdowns occurred). The 2021 class, however, was limited on interviews through their first 6 months of second-year training.
COVID-19 made it more difficult for those nephrology fellows who were contemplating going into private practice to be able to identify and interview for positions.
Instead, they stayed in place. From personal experience and conversations with several nephrology-focused recruiters, it is apparent that more fellows stayed on to do an additional year of training through transplant, critical care and interventional fellowships. In addition, some stayed in their current locations after completing training but chose to work as a hospitalist or internist (if competitive nephrology opportunities were not available locally).
Things have improved since December 2020, when vaccinations became available for physicians and health care workers. Physicians who were in practice were not constrained as much as fellows by timeframe and were able to interview and travel as lockdowns ceased and things opened up across the United States. Those who moved seemed to be fewer in number than in the period before COVID-19.
More fellows should be coming out of training programs next summer than in the last 2 years, as students doing additional years of fellowship finally complete their training. For private practice as an option, there will be an increase in opportunities available due to retirements, along with an end to hiring freezes. Likewise, physicians who were contemplating moving – but held off due to some of the reasons previously mentioned – are now ready to go. Finally, starting compensation has seen significant improvement as the shortage of candidates persists.
As a result, there will be more movement among physicians in the coming year. While this will be a positive step in fulfilling needs in the workforce, the shortage of nephrologists will continue until the specialty does more to attract residents into nephrology and, in addition, make stronger efforts to keep those who have trained in the specialty to stay in the profession.
The COVID-19 virus has tested the world’s population and economy, leading to changes in the way we deal with all aspects of life. The idea of months ahead of social distancing, mask wearing, high unemployment, business closures, new rules for eating in restaurants and limited attendance at concerts and sporting events does not bode well.
Likewise, the virus has placed an undue burden on many health care workers on the front lines. Assuming we bring the management of this virus under control, it remains unclear what impact it will have on the health care profession.
Prior to the pandemic, nephrology had already lost much of its glitter as a specialty when compared to other internal medicine subspecialties. The nephrology match program in 2020 was 62%, meaning 38% of the positions remained unfilled or were filled by candidates coming from the supplemental offer and acceptance program.1 The number of candidates filling slots has remained stable but the number of nephrologists going into private practice is continually diminishing (70.3% of fellows in 2011 vs. 51.5% in 2018).2 A significant number of international medical graduates represent 69% of fellows, but they have visa issues that require them to work in underserved areas (J-1 visa) or with an academically affiliated hospital (H1b). There also appears to be more fellows albeit a small number, who have no internal medicine training in the United States. Thus, they are ineligible to take nephrology boards.
Additionally, many nephrology fellows have an eye toward working as hospitalists or as critical care physicians due to better initial compensation, scheduling and lifestyle reasons. According to the Medscape 2020 Physician Salaries Report, nephrology has the lowest percentage of practicing physicians among all specialties (at 44%) who feel they are fairly compensated.3

With the new normal created by the novel coronavirus, what does that hold for the future of the nephrology physician work force in both the near and long term? There are several things to consider.
As mentioned, fewer physicians are going into private practice. However, it is possible this will be offset short term with the potential of fewer nephrologists retiring as planned due to recent economic volatility and its impact on 401k accounts, retirement plans and joint ventures. One need only look back at the impact on the nephrology workforce in 2008 when the recession decimated retirement nest eggs. Many of the true first wave of nephrologists had planned for retirement at that time and yet continued practicing for several additional years before they were more secure in their financial future to finally leave practice.
Currently, many nephrology practices are feeling the financial effect of diminished patient volumes and hospital consults being minimized due to stay-at-home orders and patient fears of leaving home during this time. A recent survey by the Medical Group Management Association indicated 97% of physician practices have experienced a negative financial effect directly or indirectly as a result of COVID-19. On average, practices report a 55% decrease in revenue and 60% decrease in patient volume since the beginning of the COVID-19 crisis.4 Although monthly capitated payment income and medical directorship money is still there for nephrologists, office clinic and consult income has been affected in some areas. How quickly practices recover economically (assuming there is not a recurrence) now that states are lifting this restriction and allowing elective procedures – and what impact that will have on future practice growth and need for additional physicians – has yet to be determined.
The biggest game changer potentially for nephrology, however, is the increased utilization and quick acceptance of telehealth by physicians and patients and how that will alter the nephrologist-patient relationship in the future. With CMS waiving originating site and geographic restrictions on the use of telehealth, drive time for most nephrologists has been impacted greatly as has seeing patients in the office. If the temporary reimbursement rates to nephrologists for telehealth visits remain in effect after the COVID-19 crisis dissipates, and there is good reason to believe they will based on comments made by CMS Administrator Seema Verma this trend should continue and grow.5 Getting paid at equal rates via telehealth for office and dialysis visits will alter every physician’s day and schedule. Drive time for nephrologists will be down substantially. Office visits and dialysis rounding can be done from a physician’s office or even home, further reducing drive time. With the ability to handle a greater patient load, we might see workforce in practices shrink unless there is a significant increase in the incident patient population.
The COVID-19 crisis and our response to it is rapidly changing. There is no clear-cut end in sight nor is there a way to determine the long-term effects it has had on our country and way of life. One thing is for sure. It has the potential to change the physician/patient relationship forever and the way nephrologists will practice in the future. Only time will tell us how.
PERSPECTIVE
Martin Osinski
The results of the most recent ASN/Hopkins survey among nephrology fellows are not all that surprising. Like many industries in and out of health care dealing with the desires and demands of millennials coming into the workforce for the first time, nephrology is feeling the impact. Lifestyle, according to the survey, is the overall key factor in the decision-making process for this age group when looking for that first job. Based on the results of this survey, for example, limits on weekend and weekday call rotations is the most important factor to fellows coming out of training.
While this may be the case for the fellows who responded to the survey, it is also important to note that the results may be skewed by additional factors. The authors of the report did indicate a wide variance between international medical graduates (IMGs) with student loans ($0 median) and American medical graduates ($225,000 median) who responded to the survey. It would be reasonable to expect income and debt assistance to be a priority for the American medical graduates. A large percentage of IMGs must deal with visa assistance, either with J1 or H1b visas. With 64.5% of nephrology fellows being international medical graduates who responded to the survey and 45% of them requiring visa assistance, their main focus for finding a job is going to be different as well. IMGs who are on visas have to deal with finding positions in locations that are underserved for J1 visa requirements and meet specific requirements as H1b visa candidates. Their choice of geographic locations may have to be limited in order to meet those requirements. While call rotation may be the highest factor for all nephrology fellows, the realities of student debt and meeting visa requirements creates a differing focus for many IMGs.
Location was another major factor according to the survey in choosing an opportunity; 64% of fellows indicating there were “too few” or “far too few” opportunities within 50 miles of their programs. Some of the reasons for this dissatisfaction is a result of the majority of training programs being located in nine states. It should not be surprising that more than 50% of nephrologists out of fellowship are in those states (43% of fellows completing training chose to stay within the same state of their training program sites). But a key factor that may be limiting job opportunities in those states is that the populations are not growing as rapidly as they have in the past (New York, New Jersey, Pennsylvania, Illinois and Ohio are five of the nine states; they grew 1.3% or less in population during the last 8 years vs. a national average of 6%). These slowdowns in population growth combined with the increase in physicians wanting to remain in those states makes procuring a position difficult.
Another factor that plays into the unattractive position close to the training programs is that many of those schools are in metro areas, which are highly competitive for jobs and where tax rates and cost-of-living are high. These factors all impact salaries, which in these locations are not necessarily as competitive with national averages. Between the number of opportunities available and the inadequate compensation, it forces a number of nephrology fellows to accept hospitalists or internal medicine positions in the communities where they want to stay. As a hospitalist, their initial salaries will be substantially higher than those of a first-year nephrologist and the week-on/week-off schedules can be attractive. The downside is that you are not practicing nephrology (which is the reason for going through the fellowship) and there is limited long-term growth potential.
It should also be noted that more than 48% of the respondents in the survey are in their first year of training. There is a strong possibility that their attitudes and plans may change after fellowship. There is minimum exposure during training to how to go about looking for employment. As a result, as the fellows go through their interviews, they are exposed to factors they may not have considered in responding to a survey question a year in advance and may alter their priorities and responses.
In summation, while the survey provides insight into key factors fellows utilize in determining their post fellowship plans, the results can be misleading if the motivations of the respondents are not considered.
Martin Osinski, MBA, CVA
Nephrology USA-
division of American Medical Consultants Inc.
Palmetto Bay, Florida
Nephrology News & Issues Editorial Advisory Board member
Nephrology News & Issues, May 2018
Martin Osinski, MBA, CVA
How things have changed. Twenty-five years ago, nephrology fellows coming out of training were looking for opportunities that would allow them the chance to grow a practice and they were willing to take risks. Many candidates were happy to get an income guarantee and perhaps a medical directorship to establish a new practice and let their own efforts speak for themselves.
Martin Osinski. MBA, CVA
What can we expect — and what do we think we need — to handle the kidney disease population over the next 30 years?
Having helped nephrologists, young and old, find employment over the last 30+ years, it’s my view that the specialty is at a crossroads.
By Martin Osinski, MBA, AVA
from Nephrology News & Issues
Nine years of your life.
That is the minimum number of years a fellow needs to complete post-college training to become a nephrologist. For many of you, especially those that have done training in other countries, that time frame is substantially higher. But now that it is time to look for a job in what has been a difficult market, what are your options?
from ViewPoint, Nephrology News and Issues , March 2012
by Martin Osinski
“Doctors Going Broke,” read a CNN headline on Jan. 5. Similar stories appeared in The New York Times and other national publications. One cannot say that broke is the right term for an occupation that averages in excess of $200,000 (primary care) or more than $350,000 (specialty incomes) a year, four to seven times the per capita national average. However, you only need be in practice to recognize the difficulties physicians are dealing with financially.
from Nephrology News and Issues , April 2011
by Martin Osinski
These past 15 months have represented some of the most tumultuous and difficult periods of time for physicians in practice, especially nephrologists. The number of government and economic policy changes and their immediate impact has never been greater. This left many practices unsure of taking the best steps to move forward.
This article will review the various policies that have been implemented and their impact on the average nephrology practice.
Michelle Beaver
10/2010
Renal Business Today
The numbers are daunting. Consider these statistics from the Association of American Medical Colleges graduate questionnaire and try not to glaze over and fall off your chair in a fit of depression:
Judie Bizzozero
01/14/2010
Renal Business Today
Just like the rest of the workforce, nephrologists eventually have to hang up their stethoscopes someday and enjoy life after work. However, the recent recession and a rollercoaster stock market have to hurt potential retirees and cause a them to work beyond what they planned. That's why it is important to have a solid retirement plan in place as soon as possible. This is especially true as more young nephrologists enter the workforce.
Published by the Nephrology News & Issues., January 2009
by: Martin Osinski, MBA, AVA
Practices have different options for compensation packages; VACs also offer investment opportunities
Published by the HealthLeaders Magazine., January 2009
How involved should executives be in efforts to bring docs on board?
5 years from now, the U.S. Renal Data System predicts, we will nearly double the endstage renal disease population in the United States. With the ongoing struggle to increase organ donation, most of those 650,000 individuals will be on some form of dialysis.
Ninety percent of medical groups that participated in the Cejka Search and AMGA 2005 Physician Retention Survey reported having programs to track physician turnover. That number is up from the 73% that reported doing so in 2004. Additionally, 58% of groups have designated retention-improvement initiatives, up from 48% the previous year.
By Martin Osinski
In January NN&I reported on an announcement by the Council on Graduate Medical Education (COGME) that it is predicting a shortage of physicians in the near future. COGME says that by 2015, an increase of 3,000 U.S. medical graduates, a corresponding expansion in the number of resident positions, and a change in the distribution of residency positions to more closely mirror market demand are all needed, By 2020, there could be a shortage of 85,000 physicians, they said.
Lackluster Interest Among U.S. Fellows and Government Restrictions Could Spell Disaster for Nephrology Specialty
By Martin H. Osinski and Michael J. Kirschner
Conducting a comprehensive search is an extensive, time-consuming process when you are seeking a quality physician to fit your organizational goals. You should evaluate the situation carefully. Before you initiate a search, it is critical that you are methodical, organized and efficient since the process takes commitment and is costly. This article will explain 10 steps to identify quality physicians in a reasonable time frame.
By Martin H. Osinski and Michael J. Kirschner
One of the last stages in the physician recruitment process is presenting the contract to the qualified candidate. This step should be a formality and many organizations have mastered this stage. However, for some organizations, it becomes a major obstacle. If a top quality candidate is lost at this period of the process, it becomes demoralizing. A well-designed contract can save significant time, money and avoid massive frustrations.
This article provides suggestions in designing a successful physician employment contract.